Bite Correction Appliances
Appliances in conjunction with braces are typically used with patients are not compliant with their elastics or rubber bands but also when the bite or malocclusion is significant. The determination of which type of appliance to use is dependent on the orthodontist and the severity of the bite.
Patients with a recessive lower jaw have several typical dental characteristics, the most common of which is overjet. Overjet is the relative distance in the horizontal dimension between the upper and lower front teeth. The amount of overjet will determine which appliance will be used. Typically mild to moderate overjet can be corrected with Class II elastics alone. However significant overjet may require special appliances. There are a vast number of appliances to correct overjet. At Hometown Orthodontics, Dr. Virdee will commonly use Forsus appliance, the Herbst appliance or the Headgear appliance to correct a moderate to severe Class II bite and overjet.

Forsus Appliance
The 3M Forsus springs or appliance is traditionally used as a way to correct a moderate to severe bite. It reduces the distance between the upper and lower front teeth (overjet) without using elastics. Patients like this option because it eliminates the need for compliance with elastics. The Forsus springs are typically installed 6-8 months after treatment is initiated as the patient has to be in stiff wires for the appliance to be installed. The appliance is in place for 4-6 months depending on the amount of correction that is required.
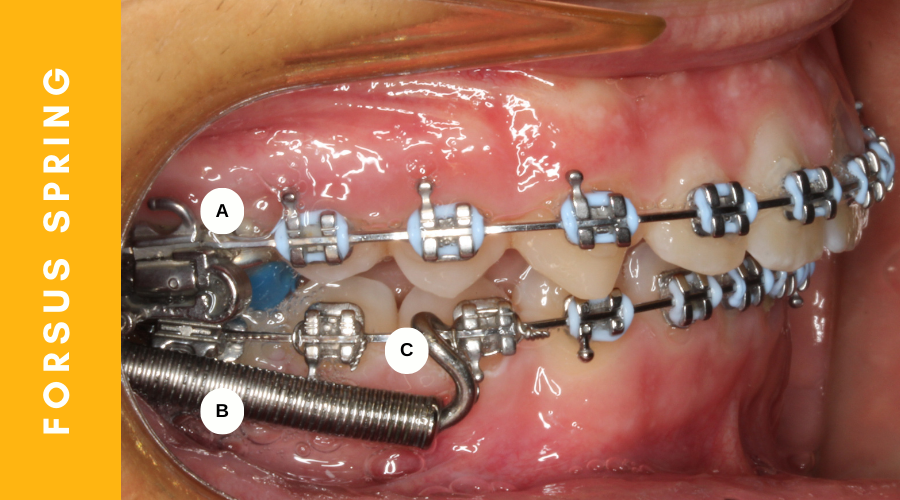
What are components of a Forsus Appliance?
The Forsus spring has two parts: A module (“B in the figure below) that attaches to the upper first molar bands (“A” in the figure below) and rods that are crimped around the lower wire( “C” in the fibure below). These molars are initially banded (“A” in the figure below) – which means that we place a ring around these teeth instead of brackets. Molar bands or rings allow for the module to be inserted into the tube with superior retention compared to a regular bracket or brace.
The Forsus module is a hollow tube so it can receive the rods that attach to the bottom wire. The rods come in various sizes and Dr. Virdee selects the size of the Forsus rods to determine which size will result in slight activation, which means that the patient will feel slight forward pressure on their lower jaw. The forward pressure stimulates growth of the lower jaw forward. Some patients tend to push their lower jaw forward until they do not feel the pressure of the springs. This is not recommended as the springs will no longer be active and adequate bite correction cannot be achieved within the desired time.
After initial insertion of the Forsus appliance, the teeth will move so that the bite starts to align. We usually see patients with the Forsus appliance every four weeks to activate the rods with a 2-3mm crimp that is placed on the rod. This compresses the module to help produce more force to gradually correct the bite to ideal standards. Dr. Virdee usually over-corrects the bite to a slight underbite by the time the appliance is removed. This an important step as the bite can relapse into a slight overjet upon removal of the appliance.
What is the Patient’s Experience with the Forsus Appliance?
Based on clinical experience, most patients do well with the Forsus springs. Patients who are not compliant with elastics are the biggest fans of the Forsus appliance. The appliance is narrow and streamlined and sits against the teeth and in mildly abuts the cheeks. Most patients get accustomed to the appliance within a week. When we see patients for their initial check up and ask them about their experience with the Forsus springs, a majority of patients tell us “It wasn’t as bad as i thought it would be.” Most patients will feel mild discomfort of their teeth just like a typical orthodontic adjustment. We recommend Advil if there is significant discomfort.
What to Expect with the Forsus Appliance
- Because the rod is inserted in the hollow module, it can sometimes come out of the module. This happens most often if a patient opens their mouth wide while yawning or laughing so that the mouth is stretched open to its maximum opening. Many patients are able to reinsert the rod back into the hallow tube of the module when this occurs.
- Irritation can sometimes occur to the inside of the cheek, just like when someone gets braces for the first time. Using wax or adding cotton rolls between the cheeks and the rods help to create a buffer zone to limit irritation until the tissues get accustomed to the new appliance.
- Brackets can break in any orthodontic patient, especially when they eat hard, sticky or chewy foods. However, because the Forsus appliance puts force on the lower brackets, sometimes this can result in increased breakage of the brackets directly adjacent to the rods. If the lower bracket does break we usually repair this by bonding dental resin to the tooth and the orthodontic wire until the appliance is ready to be removed.
[Photo of broken bracket with bonding resin applied]
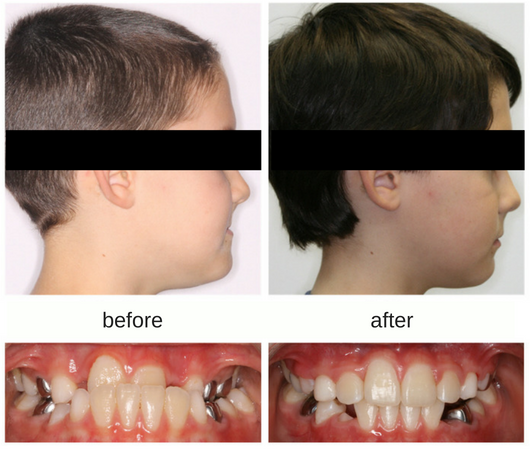
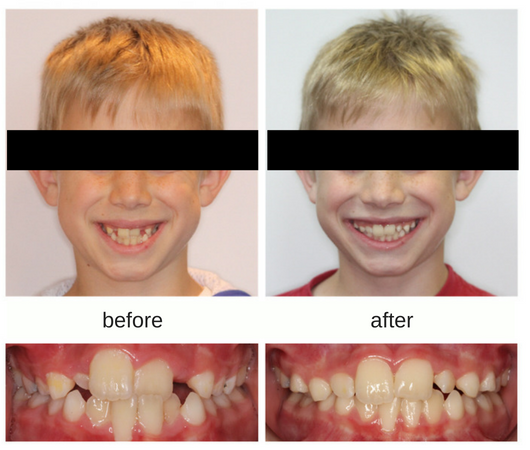
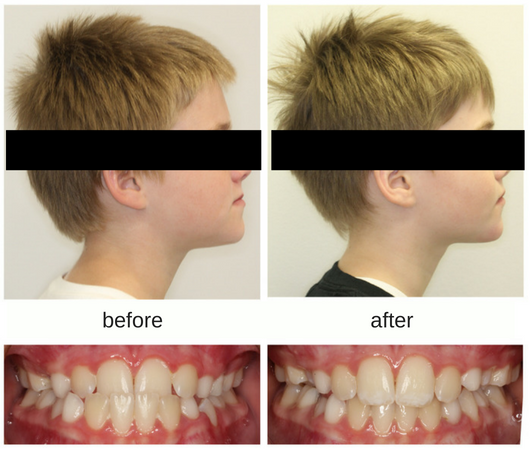
Before and After Cases with Forsus appliance
Headgear Appliance
Despite the stereotypes associated with headgear, it is one of the best appliances that you can use in growing teens! Why? Any time you correct overjet, one of two things must occur: 1) The lower arch and lower teeth can be move forward 2) The upper arch and upper teeth can be moved forward. Most class II correctors (appliances or devices that help to correct overjet) move the lower arch and lower front teeth forward. Headgear is the only appliance with the capability of helping to shift the upper teeth back.
The potential for gingival recession in orthodontics
Most patients will use elastic or rubber bands to help correct their bite without any consequences. However there are side effects to using elastics or any appliances that work by shifting the lower front teeth forward. Generally speaking, the bone that houses the lower incisors is finite and cannot be grown in the direction of the lower lip. This means that if you have initial crowding of the lower front teeth and they are aligned using braces or clear aligners like Invisalign, they will naturally move forward, closer to the edge of the bone in front of it. As teeth move, bone is resorbed (taken away) from the place that they move to. This means that you are aligning the lower incisors, you are consequently losing bone. This is ok if you have plenty of bone in front of the incisors. However if there is already thin bone, there is a risk of gingival recession. Remember, the gingiva follows the bone, so if you have bone loss, then this will naturally result in gum loss which is known as gingival recession. Gingival recession can be minor where only the cuff of the root of the lower incisors can be seen, or it can be excessive where the middle part of the root of the tooth is visible, increasing the risk for tooth mobility and potential tooth loss. While grafting can help with covering exposed roots, the bone overlying the roots of the teeth can never be replaced.
[Photo of Maria Padiuk, Patricia Dusting, Payton Rix]
In cases where the patient presents with crowded lower incisors with thin bone and large overjet that will be corrected using appliances that push the lower incisors further forward, the potential for significant recession requiring grafting is high. In growing patients, with recessive lower jaws, Dr. Virdee may recommend the Headgear as a better option in order to minimize the movement of the lower incisors forward. The risks associated with forward movement of the lower incisors is not lost on dentists! In fact, in our practice, many of the young patients who are children of dentists will prefer to wear this appliance because their parents understand the risk of moving the lower incisors out of bone and the associated consequences including bone loss, gingival recession, and the need for grafting, which is quite a painful experience.
What is the Headgear Appliance?
The components of the Headgear appliance include the facebow, neck strap and elastic modules. The facebow attaches to a tube on the band or ring that will be placed on the upper first molars. The elastic modules are attached to the neck strap are then attached to the external part of the headgear. Headgear is to be worn between 12-14h daily. The time worn does not have to be continuous. You do not have to wear headgear to school or activities with friends. We recommend wearing the headgear to bed but also when the patient is at home watching TV, doing homework or playing. Typical time to wear this appliance with braces is approximately 9-12 months. Most of the patients that we see are pretty good at wearing the appliance and can manipulate the facebow to insert and remove it themselves. We ask the patient to bring their headgear appliance at each orthodontic visit.
[Photo of Headgear]
How does Headgear work in growing patients?
Headgear helps to correct overjet in two ways. If the upper twelve year molars have not yet erupted, it will help to push the upper teeth backwards, reducing the overjet with this movement. The second, and more important movement is by helping to minimize the forward growth of the upper jaw so that the lower jaw is allowed to catch up. Remember, in growing patients, this appliance is used once the patient has started their pubertal growth spurt. This means that the patient is going through a rapid change in their hormones which allows accelerated growth of the lower jaw. The combination of jaw growth and posterior or backwards movement of the upper front teeth help to correct the overjet without excessive movement of the lower incisors which would otherwise result in flaring or forward movement of the lower incisors.
What if patients are not compliant with Headgear?
While headgear is the gold standard to help correct overjet, it requires patient compliance and not every patient is great at wearing it.
In cases where the appliance is not worn as instructed and there is still resulting overjet, we will offer the patients elastics to wear with the understanding that the potential for bone loss and gingival recession around the lower incisors increases. The chance of this occurring in patients with thin bone is greater than in those with thicker bone around the lower incisors. If Dr. Virdee finds the bone to be acceptable after initial alignment of the teeth, we may also recommend the Forsus appliance. There are ways to manipulate the appliance to help the upper molars move backwards and limit the force on the lower incisors. The last resort is ofcourse interproximal reduction (filing of the upper front teeth to reduce their proclination) or extraction of permanent teeth in the upper jaw, again to help bring the upper front teeth back in order to reduce or idealize the overjet. Dr. Virdee would do a careful evaluation of the patient to determine the best course of action.
[Before and After Photos of patients treated with HG]
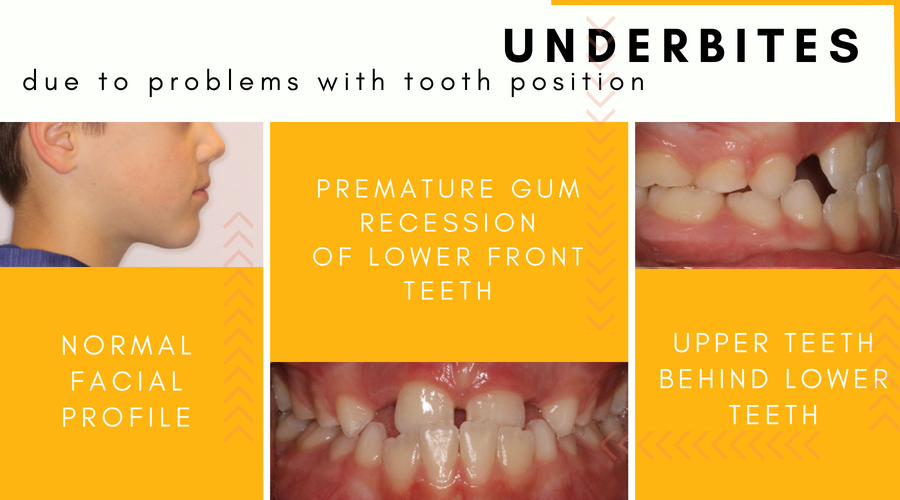
Maintaining a healthy and comfortable may be difficult when growing up with an orthodontic issue such as an underbite. Recognizing and correcting underbites is one of the reasons that orthodontists like to see patients by 7 years of age. This is the time when children are still growing and their bones are still immature. Early orthodontic treatment in young children can help to correct difficult problems such as underbites and minimize complicated issues in the future.
What is an underbite?
An underbite is a malocclusion or “poor bite” that occurs when the lower teeth and jaw protrude beyond the upper teeth and jaw. Underbites can vary in severity from being mild and barely noticeable to being severe enough that there is a distortion of facial features which may create self-esteem issues in the future.

What are the causes of an underbite?
Underbites are typically seen in 5-10% of the general population and usually have a genetic predisposition. If you or someone in your family has an underbite, the likelihood of your child developing an underbite as they grow is high. Some ethnic groups (Asian, First Nations People) are also more likely to develop underbites. Underbites can also occur or worsen due to thumb or digit sucking habits, prolonged pacifier use, a tongue trust, excessive mouth breathing and interferences between upper and lower baby or growing adult teeth.
Complications of underbites in growing children:
- Difficulty speaking, chewing and swallowing
- Poor tooth alignment
- Chronic jaw or joint (TMJ) pain, as well as head- and earaches
- Tooth decay from excessive wear of the tooth enamel
- Chronic mouth breathing, halitosis and bacterial infections
- Sleep apnea, snoring and other nighttime breathing difficulties
- Self esteem issues
How do you correct underbites in children?
Each child is unique and the cause of every child’s underbite is not the same. If steps are taken while the patient is young, the right appliance is often just the thing to resolve the problem. This highlights the importance of early orthodontic screening in children, which should be explored by the age of seven. Whether you come to our Sudbury orthodontics or Mississauga orthodontics office, Dr. Virdee will assess the cause and severity of the underbite, and determine the best course of treatment based on the age of the patient.
If the cause of the underbite is due to a problem with the position of the upper or lower front teeth, this is best corrected with limited braces or a removable retainer. However, if the cause of the underbite is due to excessive growth of the lower jaw, this is best treated with an appliance called protraction facemask in combination with a rapid palatal expander. Because your child is still growing, these appliances take advantage of a child’s natural growth potential to correct the underbite without the need for invasive surgery in the future.
How does an expander and protraction facemask correct an undebite?
A protraction facemask (also known as a reverse pull face mask) is used in combination with an upper jaw expander (rapid palatal expander) to gradually correct the underbite . The expander is inserted first and gently widens the upper jaw (see our treatment of Crossbites to read more about expanders). On the cheek side of the expander, two hooks are used to connect the facemask to the expander with elastics. The facemask rests on the forehead and the chin, which are used as anchors to gently help the upper jaw to grow forward.
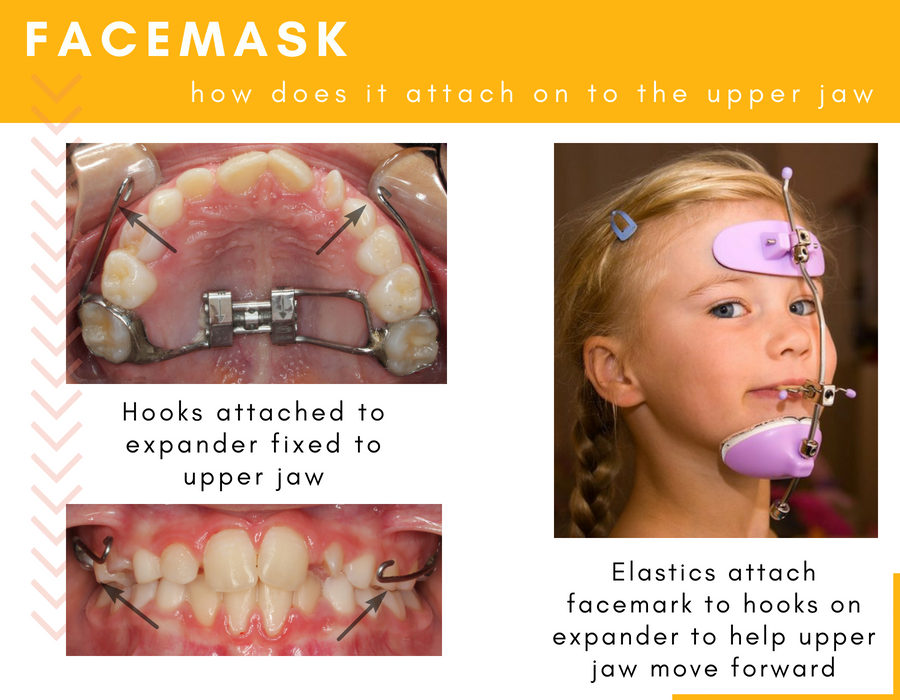
Treatment for underbite correction can range from 6 months to a year depending on your child’s growth potential, the severity of the underbite and compliance with wearing the facemask. Because the bones are less mature in younger patients, the upper jaw is easier to grow. If your child has a severe underbite, it makes sense that it will take longer to correct. The greatest predictor however of treatment success is the patient’s compliance or willingness to wear the appliance at least 12-14h per day.
Does my child wear the facemask to school?
No your child does not have to wear the facemask to school. We ask that you insert the appliance when they get back from school and while they are watching TV and doing homework, or whenever they are at home to maximize the amount of time that they are wearing the appliance. We also ask that the facemask be worn to bed.
How will the appliances used for underbite correction change my child’s day to day life?
Like anything new, your child has to get used to the expander in their mouth. The good news is, because children are more resilient than adults, it’s easier for them to adapt to something new. It usually takes about a week to get used to eating, chewing and speaking with the appliance. When you first start turning the expander, there may be pressure between the two front teeth and a possible gap may develop. We love to see this as orthodontists because this means that the expander is working. Overtime this gap usually closes on its won as the teeth move towards each other. Once facemask therapy is initiated, there may be some pressure on the chin – this is normal and is expected so don’t worry.
Are there other methods of correcting an underbite in young children?
There are other methods of correcting an underbite in young children. These appliances include the Frankle III appliance and the Chin Cup appliance.
The Frankle III appliance:
The Franklle is a removable appliance that patients can insert and remove on their own. There are several claims that this appliance will help to grow the upper jaw, but recent studies have shown that this is not the case. More often than not, the underbite is corrected by moving the teeth (which is a side-effect of this appliance).
But the underbite is corrected! What’s the difference you ask? The difference is that we didn’t take advantage of the child’s natural growth – we didn’t help the upper jaw grow which is the most important treatment modality that we can use. Remember – moving teeth is easy – but growing bone is very difficult. When you have a patient that has an underbite due to a problem with growth of the jaw bones, its important to use appliances that will address the specific problem and not mask the problem, especially when they are growing.
Chin Cup appliance:
>The chin cup appliance was used commonly in the 60s and 70s although it is seldom used today. It is a device that wraps around the chin and the top of the head to prevent further growth, movement and protrusion of the lower jaw. Again, based on recent studies, the chin cup has shown to be less effecting at doing what it was intended to do. You cannot stop growth of the lower, but you can help the upper jaw to move or grow to compensate for excessive growth of the lower jaw by using a facemask
What options does my child have if he is no longer at the stage where growth can be used to fix an underbite?
There are many patients and parents that are looking for an orthodontist in Sudbury or an orthodontist in Mississauga that can help them correct underbites. If a patient is close to puberty, treatment with a facemask will likely achieve limited results. In this case we will usually monitor their growth and proceed with treatment options based on growth that is recorded from year to year. If the patient’s underbite is mild and growth is stable where the lower jaw has not grown excessively within the last year of observation, non-surgical treatment using braces, Invisaglin or lingual braces is usually the best option. Moderate to severe underbites with prominent lower jaws often require surgical treatment to achieve desired results. An in depth discussion on surgical orthodontics can be found here.
Please click here to schedule your consultation appointment with Dr. Virdee!
Smile Gallery
-

Jason
-

Remy
-

Gavin
-

Andrew
-

Gavin
Get a Free Consultation
Make an appointment today and start your child’s journey to a healthy and beautiful smile with Hometown Orthodontics.